PCOS Pathophysiology: Types + Phenotypes
A diagnosis of PCOS can leave you feeling confused
You have been diagnosed with PCOS + trying to figure out what that means for you. Your doctor threw around words such as phenotype A or phenotype C, but health coaches and social media influencers are preaching of the four types of PCOS. It is no wonder that so many women with PCOS are lost, confused, and have no idea how to initiate their own healing journey.
Fortunately, it doesn’t have to be that way. My goal is to educate + empower women so they can be their own health advocate + take control of their health now + forever. So, let’s break it down.
In this article, we will:
Illustrate fundamental PCOS Pathophysiology
Explore PCOS mimicking androgen excess disorders
Differentiate PCOS types vs phenotypes
Analyze the role in PCOS management of types vs phenotypes
Learn the Vibrant Revival approach to PCOS management
Examine diverse genetic + Environmental factors of PCOS
Ponder PCOS as an evolutionary paradox
Pathophysiology of PCOS
The androgen excess seen in PCOS primarily results from functional ovarian hyperandrogenism (FOH). This means the cause of ovarian hyperandrogenism seems to be intrinsic + arises primarily due to increased sensitivity of ovarian theca cells to luteinizing hormone (LH), resulting in the excess of androgen production. PCOS insulin resistance + adrenal hyperandrogenism have intrinsic components to them as well and likely play a role in mixed pathophysiologies that drive PCOS symptoms for most women. Insulin resistance and adrenal androgen secretion may have intrinsic properties that drive PCOS symptoms, but they are also easily modifiable with lifestyle interventions. In the absence of native ovarian dysfunction, hyperandrogenemia from sources other than the ovaries (adrenal or peripheral sources) or severe insulin resistance disorders (type 2 diabetes) are unusual causes of hyperandrogenic anovulation and/or polycystic ovaries.
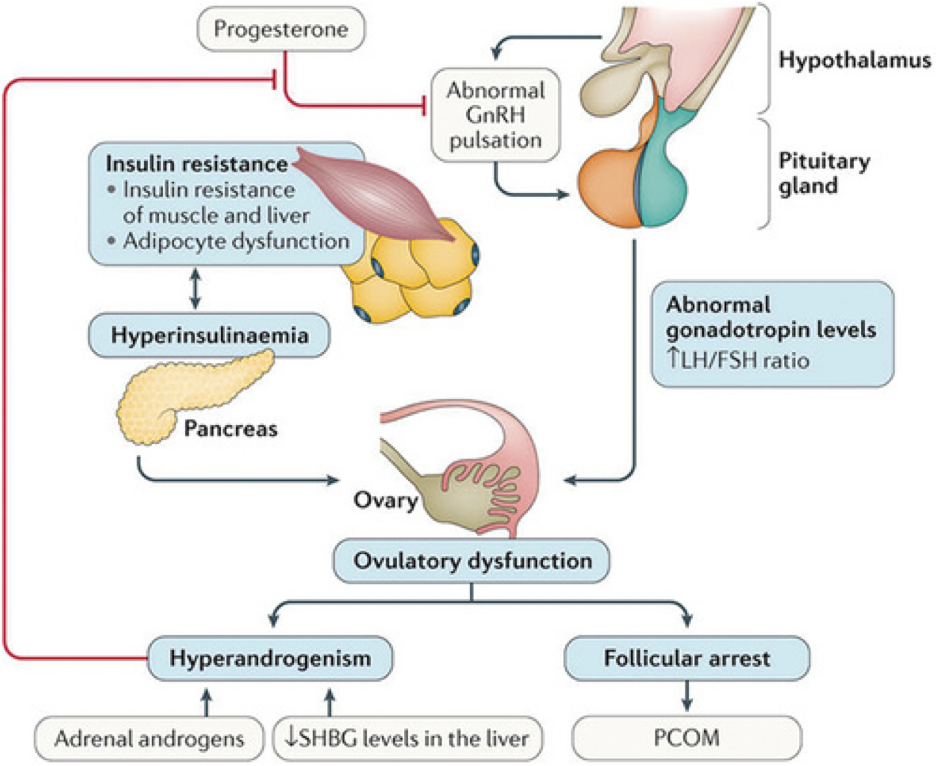
The frequency of pulsatile release of gonadotropin-releasing hormone (GnRH) from the hypothalamus is often increased in polycystic ovary syndrome (PCOS), leading to luteinizing hormone (LH) hypersecretion by the pituitary gland. LH hypersectretion + altered regulation of ovarian processes, including increased sensitivity of ovarian theca cells to LH, results in excess androgen production. Hyperinsulinemia further sensitizes ovarian theca cells to LH, leading to even more androgen production. Androgens work with follicle-stimulating hormone (FSH) to luteinize follicles by inducing LH receptors. In a healthy ovary, one dominant follicle is hyper-responsive to the luteinizing process and accumulates 10X more LH receptors than other follicles; allowing it to continue to grow while remaining follicles become growth-inhibited and are reabsorbed back into the body. Conversely, in a state of androgen excess, premature luteinization of follicles impair selection of the dominant follicle, causing follicle maturation arrest, an ovulation, + polycystic ovarian morphology (PCOM). Anovulatory cycles prevent the production of progesterone. High concentrations of progesterone are required to suppress the increased LH pulse frequency of PCOS. Low to no progesterone further promotes excess androgen production. Sex hormone-binding globulin (SHBG) is suppressed by androgens, insulin resistance + hypothyroidism, leading to increased levels of free + active testosterone. Notably, genetic, epigenetic, and environmental factors contribute considerably to the expression of these alterations.
Image borrowed with permission from Springer Nature. Nat Rev Dis Primers 2016;2:16057. Polycystic ovary syndrome, Azziz R, Carmina E, Chen Z, Dunaif A, Laven JS, Legro RS, et al. Copyright 2016.Azziz. Polycystic Ovary Syndrome. Obstet Gynecol 2018. All Content is the intellectual property of Vibrant Revival.
PCOS Phenotypes
There are three diagnostic criteria available for PCOS today. Although there are slight differences between the three, they essentially use the same symptoms. These symptoms include:
hyperandrogenism (HA)
oligo-anovulation (OA)
polycystic ovarian morphology (PCOM)
From these three symptoms, phenotypic classifications of PCOS were developed. The 1990 National Institutes of Health criteria define two phenotypes: phenotype A (HA + OA + PCOM) and phenotype B (HA + OA). Phenotype A is often referred to as the “complete” PCOS phenotype, and both phenotypes A and B are often referred to as “classic” PCOS. The Androgen Excess & PCOS Society added an additional phenotype, phenotype C (HA + PCOM), the so-called “ovulatory” PCOS. Finally, the 2003 Rotterdam criteria introduced a fourth PCOS phenotype, phenotype D (OA + PCOM), the “nonhyperandrogenic” PCOS.
Phenotypes C and D are successively less specific. Personally, I find phenotype D to be the least specific and at highest risk of capturing differential diagnosis (diagnosing PCOS when it is not), such as hypothalamic amenorrhoea. Irregular periods can be due to many different reasons and an ultrasound finding of polycystic ovaries is not specific to PCOS. Although the name of the syndrome suggests that polycystic ovaries are an important or defining feature of the syndrome, they are not. Polycystic ovaries are not unique to this syndrome. The appearance of polycystic ovaries simply means that a women did not ovulate for one month or more. It does not explain why they did not ovulate, nor does it predict their future ovulatory potential. For example, anovulatory cycles are common and normal in adolescents, but it does not predict their ability to ovulate regularly as an adult. An anovulatory cycle from time to time is also common in healthy women without PCOS. This means that polycystic ovaries can be observed in women without PCOS. In fact, one study found that healthy women without PCOS have polycystic ovaries 25% of the time (PMID2895373). The lack of hyperandrogenism in phenotype 4 makes it particularly debatable. PCOS, by definition, is a disorder of androgen excess. A diagnosis of PCOS in the absence of androgen excess is an inherent cause for concern. Observational data show that these women lack PCOS associated long term consequences which might not be communicated to women. Along with the flood of information about PCOS on social media (often of low quality), women may not be aware of their less severe phenotype and think that they have an increased risk for metabolic and cardiovascular outcomes, despite evidence demonstrating otherwise. Due to these concerns + considering that PCOS phenotypes fail to identify functional root causes of PCOS, I do not find them helpful. Determining the source/s + potential drivers of excess androgens are arguably the most important factors in successful management of PCOS.
PCOS Types
PCOS types are not based off nationally recognized society recommendations, but instead are modernized PCOS classifications based primarily on pathophysiologic drivers of PCOS. PCOS types have been described and supported by many well respected holistic and functional medicine providers and focus on a root cause approach to management of PCOS. Below, I have summarized the 4 types of PCOS.
Insulin-Resistant PCOS
Insulin resistance simply means you may have normal blood sugar, but too much insulin. Too much insulin can increase ovarian sensitivity to LH + cause your ovaries to make testosterone instead of estrogen; leading to impaired ovulation. Too much insulin also stimulates your pituitary to release more LH, which stimulates even more androgens. Finally, excess insulin lowers the androgen-binding protein SHBG. This results in more free testosterone or unbound testosterone.
Inflammatory PCOS
Inflammatory PCOS is driven by inflammation and environmental toxins. Inflammation disrupts hormone receptors and suppresses ovulation. It also stimulates both your adrenal glands and ovaries to make more androgens. Inflammation can come from insulin resistance, smoking, inflammatory foods, environmental toxins, and digestive problems.
Post-Pill PCOS
Post-Pill PCOS is a temporary surge in androgens after coming off birth control. Androgen levels can remain high for 1-2 years or more. During this time, oligo-anovulation may occur. The duration of oligo-anovulation is variable and can last from months to years.
Adrenal PCOS
Adrenal PCOS is characterized primarily by excess adrenal androgens (DHEAS). It is important to rule out other reasons for elevated DHEAS, such as high prolactin or nonclassic congenital adrenal hyperplasia (NCAH) in these situations. Adrenal PCOS is driven by an abnormal stress response system, which may be the result of stress around the time of puberty.
My main critique of PCOS types is that it paints a black + white picture + over simplifies the intricate web of root pathophysiologic features that may be contributing to your PCOS.
It is important to remember that you may have multiple drivers of your PCOS symptoms. In additional to a potential oversimplification, I personally would exclude post-pill PCOS, as I consider the surge in androgens to be a temporary withdrawal side effect of a medication and not due to an underlying intrinsic dysregulation in androgen secretion. Now, I am not saying we should erase post-pill “PCOS” from our tool box completely. Instead, I include this under differential diagnosis of PCOS. In a recent study called “Are expanding disease definitions unnecessarily labelling women with polycystic ovarian syndrome,” the authors explore the potential consequences to women of PCOS over diagnosis. Potential consequences including unnecessary treatment, stress, and worry. (PMID: 28814559) For those at risk of over diagnosis (i.e. phenotype 4, post-pill PCOS, etc) I encourage a slower, stepped approach to diagnosis to optimize benefits and reduce harm from disease labelling.
Vibrant Revivals Use of PCOS
Types + Phenotypes
As I mentioned earlier, I do not find much utilization for PCOS phenotypes in my day to day clinical practice. I do feel it is important, as a health professional, to understand the complete historical development of PCOS practice + literature so that I can serve you to the best of my ability. I also feel there can be utility in sharing this information to women with PCOS. I am a firm believer that information is power + fundamentally necessary for increased personal health advocacy. My goal is for you to feel empowered + confident to take control of your health.
Utilizing PCOS types for educational content is useful and provides important information + insight to women with PCOS. PCOS types are focused in root cause analysis and fall perfectly in line with the fundamental approach to natural + holistic care. Meaningful results from natural + holistic lifestyle interventions is dependent on appropriate identification of the source and triggers of symptoms. Clinically, I utilize an adopted form of PCOS types in my work with with women struggling from PCOS. I view PCOS as a fluid syndrome that encompasses many different combinations of driving factors contributing to the overall clinical picture. Every women is unique and deserves a detailed + in depth look into what factor/s are driving her PCOS symptoms.
Something to note
PCOS is the most common diagnosis of androgen excess, but it’s not the only diagnosis. It is important to rule out other causes of excess androgens. Other diagnoses include:
Hormonal birth control with a “high androgen index”
Psychiatric medications
High prolactin
Hypothyroidism
Cushing syndrome
Androgen-secreting neoplasms
Congenital adrenal hyperplasia
It is absolutely essential to understand and determine the source/s + drivers of PCOS androgen excess for each and every woman. As mentioned earlier, this will be the most important step in a successful healing journey for a woman with PCOS.
PCOS Genetic + Environmental Factors
A number of hereditary and environmental factors contribute to ovarian hyperandrogenism and/or insulin resistance. Polycystic ovaries, androgen levels, and insulin resistance have hereditary components. Environmental factors may be congenital or acquired and include intrauterine factors, such as androgen exposure + prenatal nutrition, and postnatal factors, such as acquired obesity + environmental toxin exposure.
Modifying risk + reversing PCOS
Yes, both genes and toxins put you at risk of PCOS, but being at risk does not mean you will always have PCOS. You can modify your genetic expression and ovarian function with diet, lifestyle, and other natural treatments—and that will improve your symptoms.
You qualify for a PCOS diagnosis based on your current symptoms. If you can reach the point of no symptoms, then you no longer have PCOS. You will always have a susceptibility. However, if you have made sustainable lifestyle interventions, a PCOS diagnosis does not have to be a part of your future.
PCOS: an evolutionary paradox
The genes that seem so disruptive in your life may have given your ancestors an advantage. PCOS developed through natural selection as a spectrum of independent, diverse genetic adaptations that evolved to preserve strength, resilience, and reproductive capacity via increased androgen and insulin production in ancient times of nutritional deprivation. Although, in current times of plenty, these genes seem to be disadvantageous.
But, here is the thing…
You can use this insight as confirmation that natural lifestyle interventions aimed to control the interaction between your external and internal environment, will be the most powerful tool on your PCOS healing journey.